Discharge management and documentation
Quality Statement 6
Before a patient leaves a healthcare facility after having anaphylaxis, they are advised about the suspected allergen, allergen avoidance strategies and post-discharge care. The discharge care plan is tailored to the allergen and includes details of the suspected allergen, the appropriate ASCIA Action Plan, and the need for prompt follow-up with a general practitioner and clinical immunology/allergy specialist review. Where there is a risk of re-exposure, the patient is prescribed a personal adrenaline injector and is trained in its use. Details of the allergen, the anaphylactic reaction and discharge care arrangements are documented in the patient’s healthcare record.
Purpose
To reduce the risk associated with a subsequent episode of anaphylaxis by ensuring that patients are equipped to recognise an allergic reaction, manage their allergy and respond to a future event, as appropriate to their clinical circumstances. All relevant information is documented to enable safe transitions of care to other clinicians involved in the patient’s care.
What the quality statement means
For patients
Before you are discharged from hospital or a healthcare service, your clinician will talk to you about the cause or ‘trigger’ for the anaphylaxis (if known), and how to manage your allergy. These triggers are also called allergens. It is important that you know the trigger for your anaphylaxis so you can avoid it. You also need to know how to recognise an allergic reaction and what to do in case of another severe allergic reaction. In some cases, your trigger may not be known and further tests may be needed.
Before you are discharged it is important that you receive:
- Information about your allergic trigger and how to avoid it
- An ASCIA Action Plan that includes information about
- How to recognise an allergic reaction including anaphylaxis. Anaphylaxis may be different each time, so it is important that you can recognise all of the symptoms
- How to use the adrenaline injector, if prescribed.
- Advice to see your general practitioner (GP) promptly, within one week.
- Information on how to arrange an appointment with a clinical immunology/allergy specialist. If this is your first anaphylaxis event, the specialist will help to confirm the cause of your anaphylaxis, and advise you about how to manage your allergy. Ask your GP to refer you to an allergy specialist as soon as possible, if arrangements are not made by the hospital. If you already have a regular specialist, arrange to see them for follow-up.
- Advice about wearing special jewellery to identify that you have an allergy.
If there is a risk of re-exposure to the trigger, you will also be given a personal adrenaline injector or a prescription for this medicine. If you are given a prescription, it is very important that you go to a pharmacy to get the adrenaline injector as soon as possible, preferably on the way home. Anaphylaxis could occur at any time and you will need to keep an adrenaline injector with you all the time. You, and your family or carer, should be trained on how to use the adrenaline injector.
If your anaphylaxis was caused by a medicine, you will be given an ASCIA Action Plan for Drug (Medication) Allergy and a record of the details of your drug allergy such as an ASCIA Record for Drug (Medication) Allergy. These will be filled out with your details. In the future, you will need to tell healthcare staff who may prescribe, or provide you with medicines, about your allergy. It is important that you know the medicine’s active ingredient name so that so you can avoid it, and that this is accurately recorded in your healthcare record.
You can also enter or update information about your allergies within your My Health Record. A guide for consumers can be found at:
nationalallergystrategy.org.au/projects/australian-digital-health-agency/consumers
You can use the ASCIA Event record for allergic reactions to make a record of the anaphylaxis event -
allergy.org.au/hp/anaphylaxis/anaphylaxis-event-record.
Information for ongoing support services available in the community, such as the Allergy & Anaphylaxis Australia information and advice line (1300 728 000), and Australasian Society of Clinical Immunology and Allergy (ASCIA) information leaflets and website will be given to you.
For clinicians
Discuss the suspected allergen with the patient and their carer and provide advice about allergy avoidance. Tailor the patient’s discharge care to the suspected allergen and risk of re-exposure to ensure adequate follow-up and preventive measures.
In most cases this will include:
- An ASCIA Action Plan
- Advice about the allergen or suspected allergen and how to avoid it
- Advice about follow-up visits with their GP and a clinical immunology/allergy specialist
- The Commission's Anaphylaxis Discharge Checklist and Discussion Guide
- Prescribing personal adrenaline injector(s), where there is a risk of re-exposure.
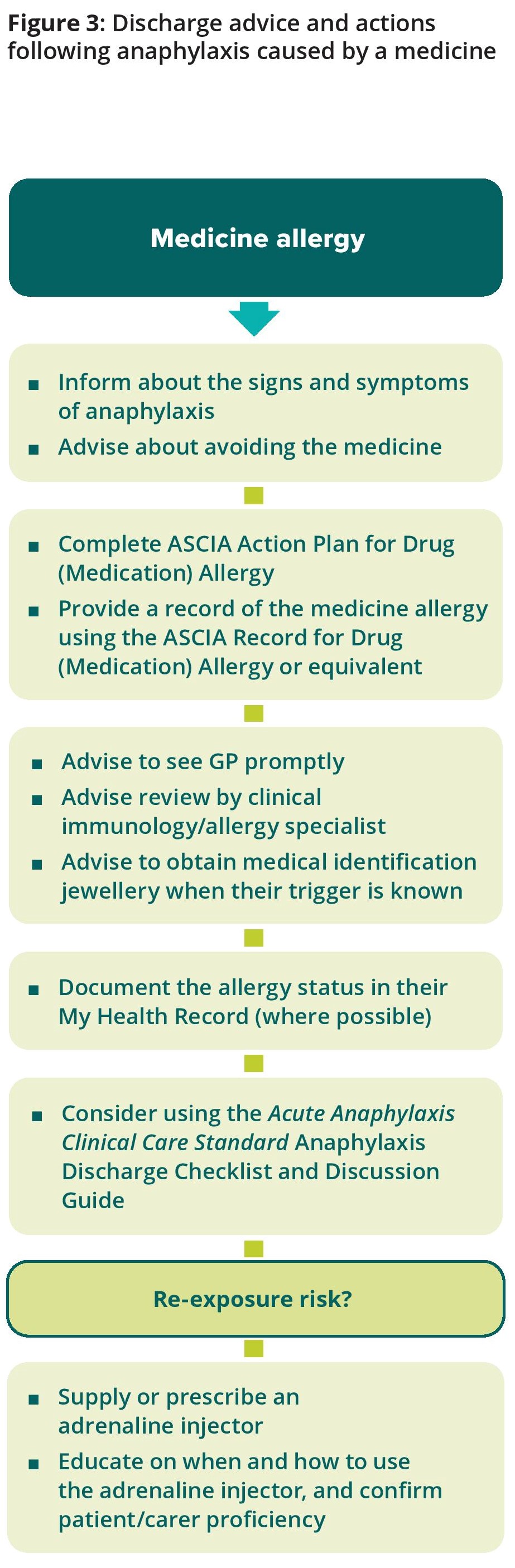
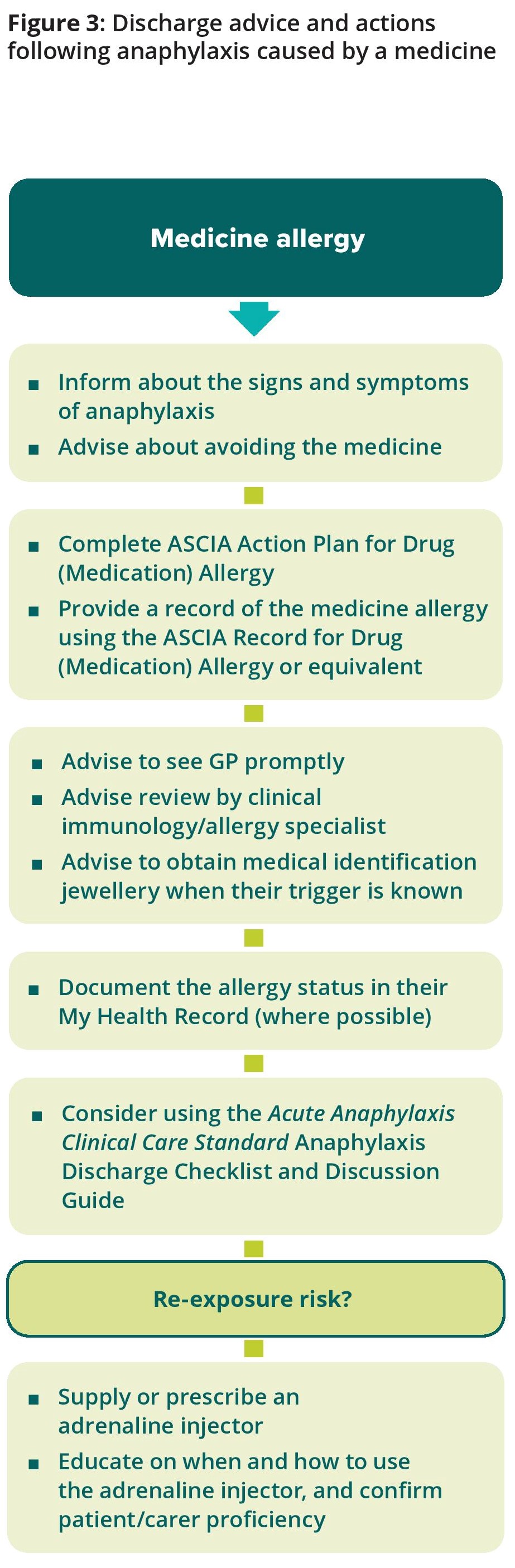
See Figures 2 & 3 for discharge requirements according to the type of allergen.
Document the allergen or suspected allergen in the patient’s health record, including food, medicine, and sting or bite exposure in the hours before anaphylaxis. For medicine allergies, include details of the adverse reaction. Upload the anaphylaxis event and their allergy status in the patient’s My Health Record when local health service arrangements allow.
Provide the discharge documents, including the suspected allergen, discharge care plan and the patient’s ASCIA Action Plan to their general practitioner or ongoing clinical provider within 48 hours of discharge. For patients with a medicine allergy, ASCIA provide a template for documenting the reaction - the ASCIA Record for Drug (Medication) Allergy. This, or a local or electronic equivalent should be completed and provided to the patient to assist patient information and clinical communication.
Recognise the degree of anxiety the patient and/or their family may experience after an anaphylaxis event. Provide the patient with information about support available in the community, such as Allergy & Anaphylaxis Australia (allergyfacts.org.au/, 1300 728 000), and the Australasian Society of Clinical Immunology and Allergy (ASCIA, allergy.org.au/patients/information).
For health service organisations
Ensure systems, policies and protocols are in place for clinicians to tailor discharge requirements to the patient’s needs and provide relevant documentation, as described in Figures 2 and 3, as appropriate to the local setting. Consider how to incorporate the tools, templates and resources described in this standard into policies, procedures and guidelines. This should include the ability to:
- Provide information on anaphylaxis and allergy management, including appropriate written patient information such as the Commission Anaphylaxis Discharge Checklist and Discussion Guide, and patient information from ASCIA and Allergy & Anaphylaxis Australia (allergyfacts.org.au/).
- Provide tailored action plans including the ASCIA Action Plan for Anaphylaxis and/or ASCIA Action Plan for Drug (Medication) Allergy.
- Document the allergic reaction and provide a record to the patient - for medicines allergies, use the ASCIA Record for Drug (Medication) Allergy or local electronic equivalent.
- Supply a personal adrenaline injector at discharge - or provide a prescription where this can be dispensed immediately upon leaving the facility - for patients at risk of re-exposure to the allergen (note: where eligible, up to two injectors may be prescribed with a PBS Authority prescription). Arranging supply of an adrenaline injector after hours may be required in some local settings.
- Provide training to patients and carers on the use of the adrenaline injector when supplied or prescribed, from staff competent to provide this training using an appropriate training device.
Ensure processes are in place for appropriate documentation of the details of the suspected allergen and the allergen exposure in the patient’s record. For medicine allergies processes for documenting and reporting details of the adverse reaction should be adhered to, including accurate documentation in the healthcare record and the discharge plan provided to the GP and other clinicians providing ongoing care. Ensure processes are in place for recording the anaphylaxis event and their allergy status in the patient’s My Health Record, when local health service arrangements allow.
Figure 2: Discharge advice - food, insect venom, or other non-medicine allergy with a risk of re-exposure
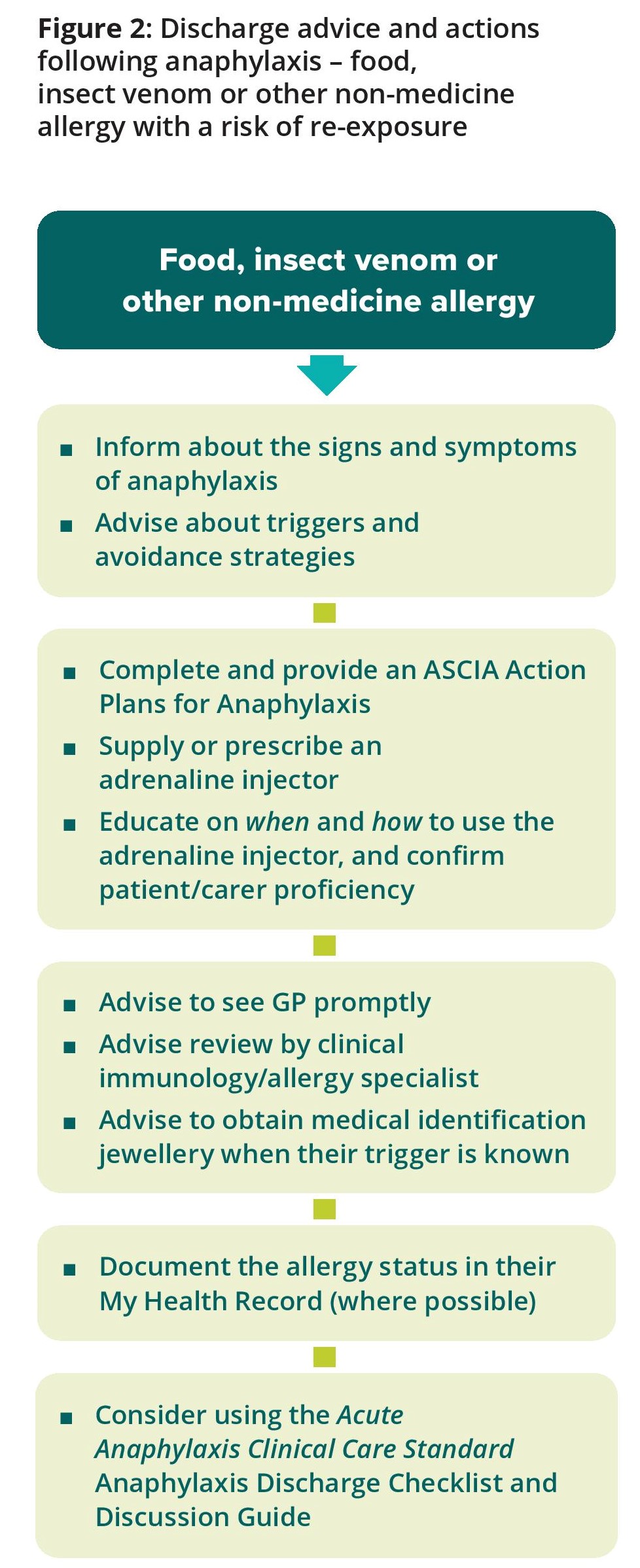
Figure 3: Discharge advice and actions following anaphylaxis caused by a medicine
For patients
Before you are discharged from hospital or a healthcare service, your clinician will talk to you about the cause or ‘trigger’ for the anaphylaxis (if known), and how to manage your allergy. These triggers are also called allergens. It is important that you know the trigger for your anaphylaxis so you can avoid it. You also need to know how to recognise an allergic reaction and what to do in case of another severe allergic reaction. In some cases, your trigger may not be known and further tests may be needed.
Before you are discharged it is important that you receive:
- Information about your allergic trigger and how to avoid it
- An ASCIA Action Plan that includes information about
- How to recognise an allergic reaction including anaphylaxis. Anaphylaxis may be different each time, so it is important that you can recognise all of the symptoms
- How to use the adrenaline injector, if prescribed.
- Advice to see your general practitioner (GP) promptly, within one week.
- Information on how to arrange an appointment with a clinical immunology/allergy specialist. If this is your first anaphylaxis event, the specialist will help to confirm the cause of your anaphylaxis, and advise you about how to manage your allergy. Ask your GP to refer you to an allergy specialist as soon as possible, if arrangements are not made by the hospital. If you already have a regular specialist, arrange to see them for follow-up.
- Advice about wearing special jewellery to identify that you have an allergy.
If there is a risk of re-exposure to the trigger, you will also be given a personal adrenaline injector or a prescription for this medicine. If you are given a prescription, it is very important that you go to a pharmacy to get the adrenaline injector as soon as possible, preferably on the way home. Anaphylaxis could occur at any time and you will need to keep an adrenaline injector with you all the time. You, and your family or carer, should be trained on how to use the adrenaline injector.
If your anaphylaxis was caused by a medicine, you will be given an ASCIA Action Plan for Drug (Medication) Allergy and a record of the details of your drug allergy such as an ASCIA Record for Drug (Medication) Allergy. These will be filled out with your details. In the future, you will need to tell healthcare staff who may prescribe, or provide you with medicines, about your allergy. It is important that you know the medicine’s active ingredient name so that so you can avoid it, and that this is accurately recorded in your healthcare record.
You can also enter or update information about your allergies within your My Health Record. A guide for consumers can be found at:
nationalallergystrategy.org.au/projects/australian-digital-health-agency/consumers
You can use the ASCIA Event record for allergic reactions to make a record of the anaphylaxis event -
allergy.org.au/hp/anaphylaxis/anaphylaxis-event-record.
Information for ongoing support services available in the community, such as the Allergy & Anaphylaxis Australia information and advice line (1300 728 000), and Australasian Society of Clinical Immunology and Allergy (ASCIA) information leaflets and website will be given to you.
For clinicians
Discuss the suspected allergen with the patient and their carer and provide advice about allergy avoidance. Tailor the patient’s discharge care to the suspected allergen and risk of re-exposure to ensure adequate follow-up and preventive measures.
In most cases this will include:
- An ASCIA Action Plan
- Advice about the allergen or suspected allergen and how to avoid it
- Advice about follow-up visits with their GP and a clinical immunology/allergy specialist
- The Commission's Anaphylaxis Discharge Checklist and Discussion Guide
- Prescribing personal adrenaline injector(s), where there is a risk of re-exposure.
See Figures 2 & 3 for discharge requirements according to the type of allergen.
Document the allergen or suspected allergen in the patient’s health record, including food, medicine, and sting or bite exposure in the hours before anaphylaxis. For medicine allergies, include details of the adverse reaction. Upload the anaphylaxis event and their allergy status in the patient’s My Health Record when local health service arrangements allow.
Provide the discharge documents, including the suspected allergen, discharge care plan and the patient’s ASCIA Action Plan to their general practitioner or ongoing clinical provider within 48 hours of discharge. For patients with a medicine allergy, ASCIA provide a template for documenting the reaction - the ASCIA Record for Drug (Medication) Allergy. This, or a local or electronic equivalent should be completed and provided to the patient to assist patient information and clinical communication.
Recognise the degree of anxiety the patient and/or their family may experience after an anaphylaxis event. Provide the patient with information about support available in the community, such as Allergy & Anaphylaxis Australia (allergyfacts.org.au/, 1300 728 000), and the Australasian Society of Clinical Immunology and Allergy (ASCIA, allergy.org.au/patients/information).
For health service organisations
Ensure systems, policies and protocols are in place for clinicians to tailor discharge requirements to the patient’s needs and provide relevant documentation, as described in Figures 2 and 3, as appropriate to the local setting. Consider how to incorporate the tools, templates and resources described in this standard into policies, procedures and guidelines. This should include the ability to:
- Provide information on anaphylaxis and allergy management, including appropriate written patient information such as the Commission Anaphylaxis Discharge Checklist and Discussion Guide, and patient information from ASCIA and Allergy & Anaphylaxis Australia (allergyfacts.org.au/).
- Provide tailored action plans including the ASCIA Action Plan for Anaphylaxis and/or ASCIA Action Plan for Drug (Medication) Allergy.
- Document the allergic reaction and provide a record to the patient - for medicines allergies, use the ASCIA Record for Drug (Medication) Allergy or local electronic equivalent.
- Supply a personal adrenaline injector at discharge - or provide a prescription where this can be dispensed immediately upon leaving the facility - for patients at risk of re-exposure to the allergen (note: where eligible, up to two injectors may be prescribed with a PBS Authority prescription). Arranging supply of an adrenaline injector after hours may be required in some local settings.
- Provide training to patients and carers on the use of the adrenaline injector when supplied or prescribed, from staff competent to provide this training using an appropriate training device.
Ensure processes are in place for appropriate documentation of the details of the suspected allergen and the allergen exposure in the patient’s record. For medicine allergies processes for documenting and reporting details of the adverse reaction should be adhered to, including accurate documentation in the healthcare record and the discharge plan provided to the GP and other clinicians providing ongoing care. Ensure processes are in place for recording the anaphylaxis event and their allergy status in the patient’s My Health Record, when local health service arrangements allow.
Figure 2: Discharge advice - food, insect venom, or other non-medicine allergy with a risk of re-exposure
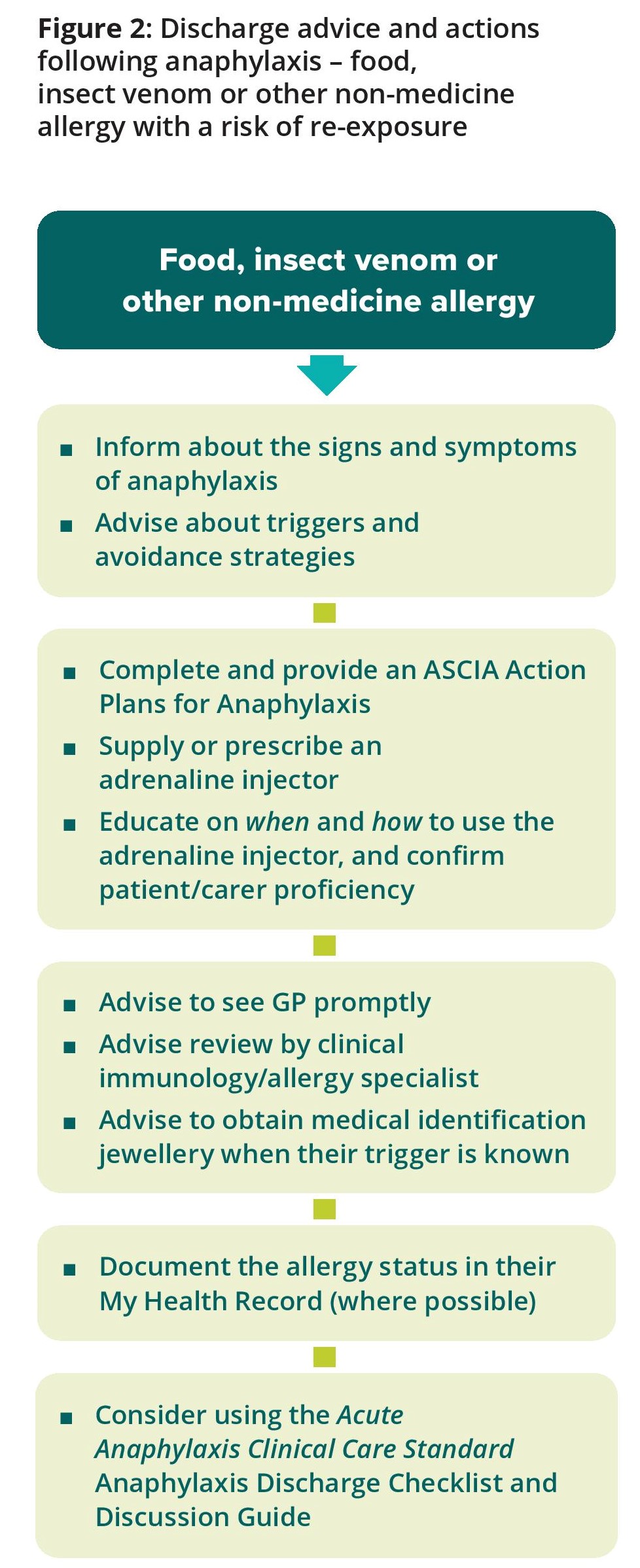
Figure 3: Discharge advice and actions following anaphylaxis caused by a medicine
Quality statement 6 has indicators for local monitoring
