Australians are unwittingly being exposed to increased risk of harm from taking antibiotics, when often these medicines are used to treat common infections where they will have no or little benefit, according to the Australian Commission on Safety and Quality in Health Care (the Commission).
Today the Commission released a state-of-the-nation report on antibiotic use and resistance, which reveals Australia ranks among the highest in the developed world for antimicrobial use.
AURA 2023: Fifth Australian report on antimicrobial use and resistance in human health highlights several dangerous bacteria as major healthcare problems because they are increasingly resistant to common antibiotics – making it more difficult to treat serious infections.
Each year hundreds of people in Australia die because of drug-resistant infections[i], known as antimicrobial resistance, which is greatly worsened by misuse and overuse of antimicrobials. Globally, WHO estimates that antimicrobial resistance could result in up to 10 million deaths each year by 2050.
The good news is that there has been an overall drop in Australia’s antimicrobial use in recent years.
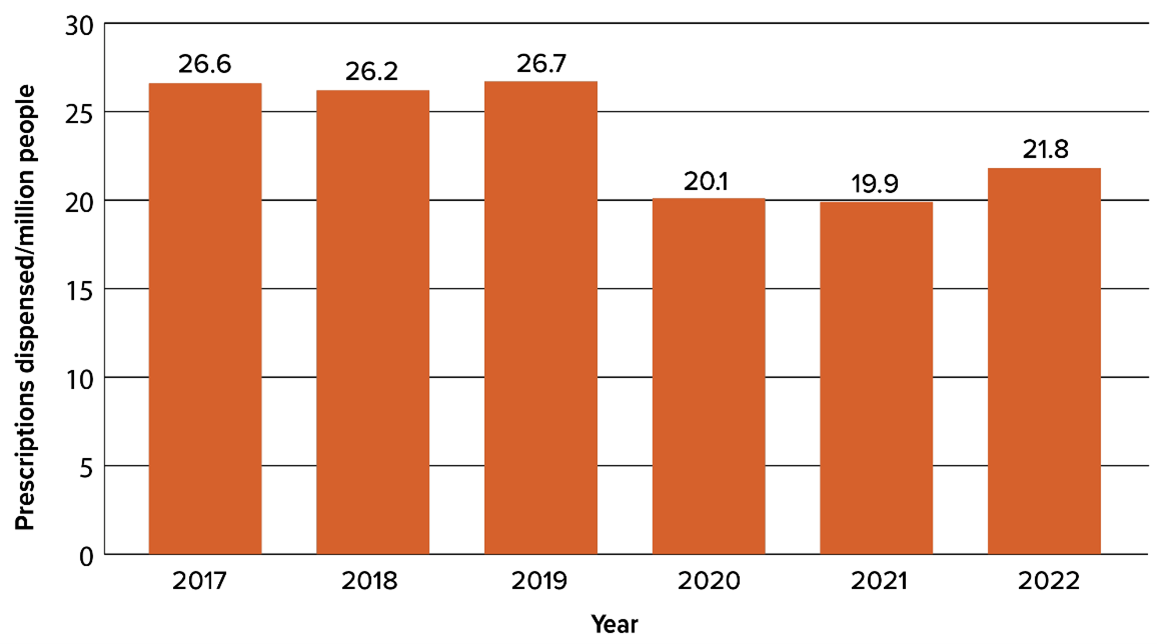
The report found that last year, 21.8 million prescriptions for antimicrobials were dispensed in the community, down from 26.6 million in 2017. One in three Australians (9.8 million people) had at least one antibiotic dispensed. This is higher than many similar countries and there is room for improvement.
Australia continues to have one of the highest antimicrobial community prescribing rates in the developed world. We rank seventh highest compared with European countries, the United Kingdom and Canada in our use of antimicrobials in the community.[ii] Australian hospital antimicrobial use is estimated to be nearly three times that of the European country with the lowest use, the Netherlands.[iii]
Encouragingly, since 2019 Australia’s antimicrobial use in the community has fallen 18% overall; with a significant 25% decline in 2020 and 2021, but a recent 10% uptick in 2022.[iv] Last year, antimicrobial use was highest in Queensland, New South Wales and Victoria.[v]
There are several reasons for the fall in antimicrobial use. These include policy changes in 2020[1], and physical distancing restrictions to reduce the spread of COVID-19 that led to a decrease in respiratory tract infections.
Professor John Turnidge AO, Senior Medical Advisor for the Commission, said the AURA 2023 findings were heartening, but we needed sustained changes in the coming years to preserve the value and potency of antibiotics.
“COVID-19 had a major impact, as it was the first time the slow downward trend in antimicrobial prescribing was significantly accelerated with the help of GPs, who did not prescribe as many antibiotics. We have an opportunity to build on this achievement to tackle one of the most serious health challenges of our time,” he said.
“AURA 2023 highlights the need to get smarter about our prescribing of antimicrobials. In the community and in aged care homes, we can ensure that prescribing for urinary tract infections, skin infections, chronic obstructive pulmonary disease and other respiratory infections is based on guidelines. Everyone has a role to play in this – doctors and other healthcare workers, as well as patients.
“In hospitals, we need to focus on appropriate use of antibiotics for surgical prophylaxis, manage the increase in organisms resistant to last-line antimicrobials such as carbapenemase-producing Enterobacterales (CPE), and monitor for emerging antifungal resistance.
“Let’s all think twice before automatically prescribing and using antibiotics – or having them ‘just in case’.
“If we don’t, in the future we may not be able to perform medical procedures such as organ transplants, cancer chemotherapy, diabetes management and major surgery. That is a bleak future that none of us wish to contemplate,” Professor Turnidge added.
Benefits of antibiotics must outweigh adverse effects
According to Professor Peter Collignon AM, Senior Medical Advisor for the Commission, more effort is needed to prevent infections and build broad awareness of the risk of harm from antimicrobials.
“The more you can do to prevent infections and avoid spreading them, the better off you, your friends and family will be – and you’ll use fewer antibiotics because you won’t need them,” he said.
“We will all be better off if we continue good hygiene habits established during COVID-19, such as washing our hands and not mingling with others when we are sick.
“Antimicrobial medications are marvellous, but there can be adverse effects. About 5% of people may experience vomiting, diarrhoea, or dizziness – while there may be zero chance of the antibiotic helping you get better if you are treating a virus such as a cold or flu.
“Ultimately, the benefits must outweigh the side effects. For a serious infection such as meningitis, pneumonia or sepsis, you will need antibiotics to stay alive and your doctor will help you navigate this. Yet for many people dealing with non-serious illnesses, this is not the case,” Professor Collignon said.
While national rates of resistance for many organisms have not changed substantially since 2019, there are several changes in rates and patterns of resistance and the sources of infections that are important considerations for infection prevention and control.
AURA 2023 highlights that antimicrobial resistance poses an ongoing health risk, with common pathogens such as Staphylococcus aureus (S. aureus), Escherichia coli (E. coli) and Neisseria gonorrhoeae (N. gonorrhoeae) increasingly resistant to major drug classes, and some organisms resistant to last-resort treatments, such as CPE.
AURA 2023 also highlights several specific types of bacteria that are key emerging issues for antimicrobial resistance, including community-acquired methicillin-resistant Staphylococcus aureus (MRSA), E. coli and Clostridioides difficile infection (CDI).
Professor Turnidge warned: “Antimicrobial resistant germs pose an alarming health risk because in more serious cases when the drugs don’t work, there may be no antibiotic options left for some patients.
“Individual risks should also be considered, including the impact on the gut microbiome and emerging evidence that antimicrobial use may contribute to long-term chronic illness later in life,” he said.
“Antibiotics can save your life, so we should preserve them to treat life-threatening conditions – but we must not forget that they can also cause significant harm.”
Next week is World AMR Awareness Week, 18–25 November. There is no better time to remind people of the risk of overusing antibiotics and the importance of good hygiene habits to prevent infections.
Access the full report: safetyandquality.gov.au/aura2023