AS 5369:2023 Reprocessing of reusable medical devices and other devices in health and non-health related facilities specifies the requirements for the effective and safe reprocessing, storage, handling, and transportation of reusable medical devices (RMDs) and other devices used in human health care and other treatments.
AS 5369:2023 is the national standard used by health service organisations to inform implementation of Action 3.13. AS 5329 supersedes AS/NZS 4815:2006 Office-based health care facilities - Reprocessing of reusable medical and surgical instruments and equipment, and maintenance of the associated environment. The Commission has developed a resource to assist in conducting a gap analysis to identify key changes and updated requirements between AS/NZS 4815:2006 and AS 5369:2023.
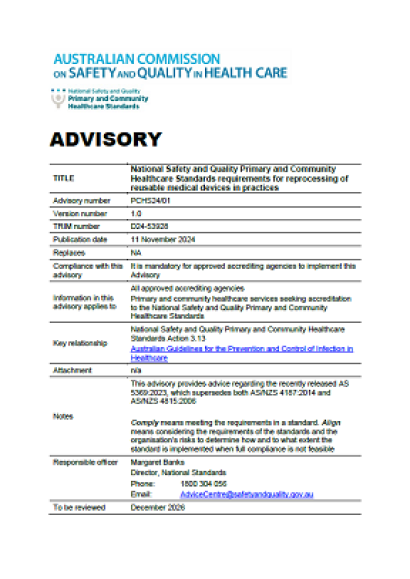
Advisory details
| Item | Details |
|---|---|
| Advisory number | PCHS24/01 |
| Version number | 1.0 |
| TRIM number | D24-53928 |
| Publication date | 11 November 2024 |
| Replaces | NA |
| Compliance with this advisory | It is mandatory for approved accrediting agencies to implement this Advisory |
| Information in this advisory applies to |
|
| Key relationship | National Safety and Quality Primary and Community Healthcare Standards Action 3.13 Australian Guidelines for the Prevention and Control of Infection in Healthcare |
| Attachment | N/A |
| Notes |
This advisory provides advice regarding the recently released AS 5369:2023, which supersedes both AS/NZS 4187:2014 and AS/NZS 4815:2006.
|
| Responsible officer | Margaret Banks Director, National Standards Phone: 1800 304 056 Email: AdviceCentre@safetyandquality.gov.au |
| To be reviewed | December 2026 |
Purpose
To describe the minimum requirements for primary and community healthcare services to comply with Action 3.13 of the National Safety and Quality Primary and Community Healthcare Standards.
Issue
Action 3.13 of the Primary and Community Healthcare (PCH) Standards states:
Where reusable equipment, instruments and devices are used, the healthcare service has:
- Processes for reprocessing that are consistent with relevant national and international standards, in conjunction with manufacturers’ guidelines
- A process for critical equipment, instruments, and devices that is capable of identifying the:
- patient
- procedure
- reusable equipment, instruments and devices that were used for the procedure
- Processes to plan and manage reprocessing requirements and additional controls for novel and emerging infections.
In December 2023, AS 5369:2023 Reprocessing of reusable medical devices and other devices in health and non-health related facilities superseded AS/NZS 4815:2006 Office-based health care facilities - Reprocessing of reusable medical and surgical instruments and equipment, and maintenance of the associated environment and AS/NZS 4187:2014 Reprocessing of reusable medical devices in healthcare services. AS 5369:2023 does not include timeframes for compliance.
AS 5369:2023 specifies the requirements for the effective and safe reprocessing, storage, handling, and transportation of reusable medical devices (RMDs) and other devices used in human health care and other treatments.
AS 5369:2023 is the national standard used by health service organisations to inform implementation of Action 3.13.
To support transition arrangements, the Commission has developed a resource to assist in conducting a gap analysis to identify key changes and updated requirements between AS/NZS 4815:2006 and AS 5369:2023.
Requirements
Perform a gap analysis
Healthcare services using critical and semi-critical RMDs and other devices that require reprocessing, are to undertake a gap analysis against AS 5369:2023 to determine compliance with the national or international standards for reprocessing of reusable medical devices.
At assessment, assessors are to ensure a gap analysis is completed by the commencement of the second accreditation assessment cycle to the PCH Standards and that implementation has commenced on an action plan.
Implement risk mitigation
Where risks are identified, risk mitigation strategies must be implemented and routinely monitored and reported to the relevant clinical governance body or individual.
This includes risks related to:
- Segregation of clean and dirty activities
- Storage of reprocessed medical devices
- Cleaning, disinfecting and sterilising equipment.
When assessing Action 3.13, assessors will confirm that a risk assessment has been conducted; there is routine monitoring and actions have been taken to mitigate identified risks. Strategies being implemented should progress an organisation towards full compliance with the national or international standards for reprocessing of reusable medical devices.
Compliance with national or international standards for reprocessing of reusable medical devices
Where risks are identified that cannot be addressed through risk mitigation processes, healthcare services are expected to work towards full compliance with national or international standards for reprocessing of reusable medical devices.
In consultation with relevant state and territory health department or regulator, healthcare services must develop a plan for meeting full compliance that includes realistic and achievable timeframes to align its requirements with national or international standards, manufacturers’ guidelines and the current edition of the Australian Guidelines for the Prevention and Control of Infection in Healthcare.
Whenever a new healthcare service commences operations, the healthcare service must align its processes, equipment and facility for reprocessing of medical equipment and devices with national or international standards for reprocessing of reusable medical devices, manufacturers’ guidelines, the current edition of the Australian Guidelines for the Prevention and Control of Infection in Healthcare and relevant jurisdictional requirements.
At assessment, assessors are to review evidence the healthcare service has a plan that includes realistic and achievable timeframes to comply with national or international standards reprocessing of reusable medical devices, manufacturers’ guidelines, the current edition of the Australian Guidelines for the Prevention and Control of Infection in Healthcare and relevant jurisdictional requirements.
Replacement of equipment
The risk of infection and manufacturers’ guidelines and instructions should inform the timeline for declaring equipment, devices and water filtration equipment inoperable or obsolete. The economically useful life of reprocessing equipment and devices and water filtration systems is to be detailed in the healthcare service’s asset register. Decommissioning and replacement of equipment is a matter for healthcare services to consider as part of their capital and risk governance.
Healthcare services replacing inoperable or obsolete reprocessing or water filtration equipment are to ensure replacement equipment addresses infection risks identified by the healthcare service and complies with the relevant national or international standards.
Where reprocessing equipment is replaced with previously used equipment, the replacement equipment should operate as originally intended and conform with national or international standards for reprocessing of reusable medical devices, the current edition of the Australian Guidelines for the Prevention and Control of Infection in Healthcare and relevant jurisdictional requirements.
At assessment, assessors are to review evidence that replaced reprocessing equipment complies with the national or international standard.
Water Quality
Healthcare services are to conduct a risk assessment and monitor water quality, in line with equipment manufacturers’ and service providers’ recommendations, to determine whether water as supplied is of a suitable quality.
Healthcare services should:
- Monitor water quality taking into consideration the requirements in AS 5369:2023 and manufacturers’ recommendations
- When determining the most suitable water treatment options, healthcare services should conduct a risk assessment guided by requirements in AS 5369:2023 and manufacturers’ recommendations.
At assessment, assessors are to review evidence that a risk assessment of water quality has been conducted, is routinely monitored and action taken when necessary to minimise risks.
Action 3.13 is to be rated:
- ‘not met’ if a gap analysis is not complete by July 2025, if the action plan is not being implemented in line with the timeframes specified in the action plan, and/or ongoing monitoring specified in this Advisory is not evident.
- ‘met with recommendations’ when there is evidence that:
- A gap analysis is underway in the first assessment cycle, or a gap analysis has been completed by the commencement of the second assessment cycle and an action plan is being implemented
- Risks are routinely monitored and mitigation strategies are in place
- Compliance aligns with the requirements of this Advisory.
Where timelines for implementation exceed 3 years, healthcare services may apply to the Commission for an extension. The link to applications for extension is here. An extension supports Action 3.17 to be rated ‘met with recommendations’ across assessment cycles.
- ‘met’ when the healthcare service have systems and processes for reprocessing of reusable medical devices that is fully aligned with the requirements of AS 5369:2023.