Step 3.4 – Translate AHPEQS data into improvement
Outcome: By completing Step 3.4 you will be able to develop ideas for translating AHPEQS results into actions that support quality and safety improvement in your services
Things to consider
This page lists the items that need to be considered in Step 3.4 to translate AHPEQS data into improvement.
Moving from survey data to practical improvement
The claim that doing patient experience surveys and collecting patient feedback will lead to improvements in services relies on several assumptions. One study identified three assumptions:
- Assumption 1 – There are valid ways of measuring the healthcare experiences of patients for use in feedback
- Assumption 2 – Feedback of information about patients’ experiences to service providers (directly or indirectly via public reporting) stimulates improvement efforts within individuals, teams and organisations
- Assumption 3 – Improvement efforts initiated by organisations, teams or individuals lead to improvement in future patients’ experiences of care.
This step is concerned with assumptions 2 and 3. What makes it more likely that AHPEQS can be used to achieve meaningful change in services? What are the conditions and actions that need to be put in place to get from a patient filling out the survey to improvements in quality and safety that are noticeable to a patient? Researchers have identified some of the barriers and enablers of the meaningful use of patient experience (and safety and quality) data.
Consumer factors influencing collection of meaningful data
A study by De Brún et al. points out that there is no likelihood of getting meaningful patient experience data if patients do not see the point of providing it, do not feel empowered to provide it, or if it is difficult for them to fill out the survey. They developed a model of barriers and facilitators for consumers providing their feedback on the safety of the service they used.
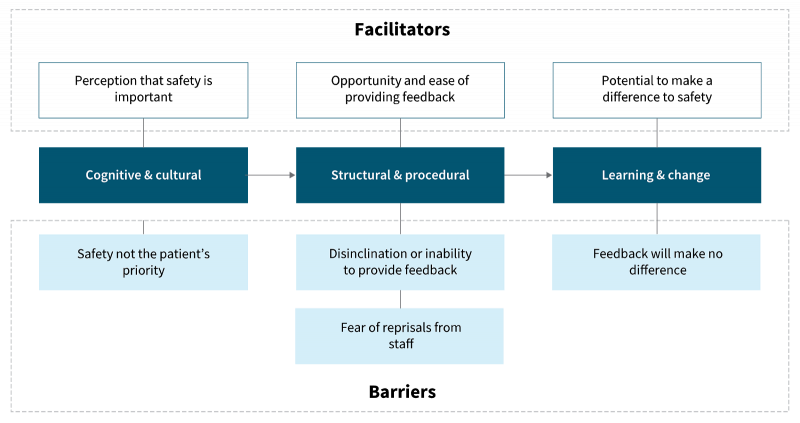
Source: De Brún et al. (2017)
Factors affecting staff use of data for improvement
Research in the United Kingdom found that healthcare staff often find it difficult to make use of patient survey data. The research highlighted the complexity of the process needed to get from the point where staff receive patient feedback to the point where they respond to it by making changes to improve safety and quality. Required conditions are that:
- Staff must exhibit the belief that ‘listening to patients is a worthwhile exercise’
- Local teams need ‘adequate autonomy, ownership and resources to enact change’
- Where high level or inter-departmental support is required, there must be ‘organisational readiness to change’.
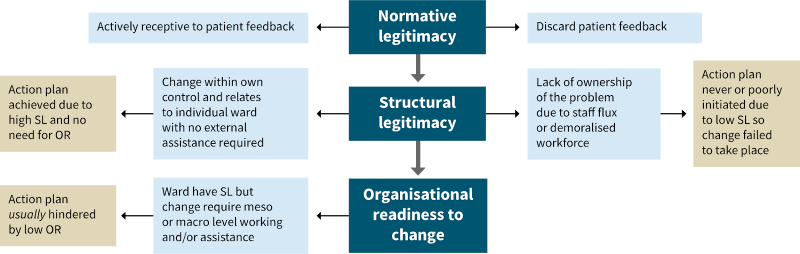
OR = organisational readiness; SL = structural legitimacy
Source: Sheaff et al. (2002)
Organisational and cultural factors influencing meaningful use of data
A literature review examined how large-scale patient experience survey results are used at a local level. They showed that translating these results into effective action and improvement depends on the following organisational and cultural factors:
- Sufficient resources in terms of knowledge, time and personnel to produce and present good quality data
- Positive attitude of staff towards patient experience information
- Effective and tailored presentation of results to staff – not just written feedback
- Common engagement and understanding from all professions in an organisation
- High-quality data collection and analysis methods, easily understood results, system to follow up results.
Davies and Cleary also identified the factors affecting the use of patient survey data in quality improvement. Although dated, this study presents a useful summary of barriers and enablers to the translation of survey data into practical change. These included:
- organisational barriers
- competing priorities
- lack of supporting values for patient-centred care
- lack of quality improvement infrastructure
- organisational promoters
- developing a culture of patient centredness
- developing quality improvement structures and skills
- persistence of quality improvement staff over many years
- professional barriers
- clinical scepticism
- defensiveness and resistance to change
- lack of staff selection, training and support
- professional promoters
- clinical leadership
- selection of staff for their ‘people skills’
- structured feedback of results to teams or individuals
- data-related barriers
- felt lack of expertise with survey methods
- lack of timely feedback of results
- lack of specificity and discrimination
- uncertainty over effective interventions or rate of changes
- lack of cost-effectiveness of data collection.
Integrated workflows
When setting up an electronic interface to present AHPEQS results within the organisation (whether this is retrospective or real-time information), consider building in workflows to make it easier to act on the results. For example, when one of the trigger thresholds developed earlier in this stage is reached, particular actions could be prompted and monitored for completion. Another way to integrate quality improvement into the workflow is to provide suggestions for action in different parts of the organisation, even where trigger thresholds are not reached – and even if the results are mostly very good overall.
Analysis and reporting of results can be part of an automated electronic workflow consisting of:
1 Identification of consenting patients in patient administration systems
2 Extraction of eligible patient demographics from patient administration systems
3 Distribution of the survey to eligible patients
4 Entry of returned responses into database
5 Quality checking and cleaning of data
6 Scoring of data
7 Descriptive statistics generation
8 Application of any relevant statistical tests
9 Presentation and reporting of results to different audiences (including live dashboards).
Feedback to consumers
It is good (though rare) practice to demonstrate to consumers who have taken the time to fill out a survey that their time has been well spent. Some options for doing this include:
- Presenting ‘real life’ evidence of previous or ongoing improvements stimulated or informed by patient experience survey results (either when sending the survey or after receiving a completed response)
- Asking consumers if they would be willing to share their experiences with frontline staff in a staff meeting or training
- Using consumer focus groups to further investigate a pattern in AHPEQS data – to get to the reasons behind a problem and to help with designing solutions.
Engaging consumers as partners with frontline staff in reviewing AHPEQS results in workshop environments to design improvements is a way to take the feedback and learning loop to a more meaningful level. Resources for experience-based co-design are available from the Point of Care Foundation.
Communities of practice
Setting up a regular forum for interested consumers, staff, managers and the executive to review AHPEQS results together is a way to ensure that all stakeholders collaborate to achieve patient-focused safety and quality improvement. This could be a virtual or face-to-face community of practice inviting consumer and frontline staff input to identify, design, record and evaluate changes to processes, structures and practices. An example of a data-driven collaborative learning model, using a different type of healthcare data, can be seen in the work of Nelson et al.
