National Standards
National Model Clinical Governance Framework
The National Model Clinical Governance Framework provides a consistent national framework for clinical governance that is based on the National Safety and Quality Health Service Standards.
To support the delivery of safe and high-quality care for patients and consumers, the Australian Commission on Safety and Quality in Health Care has developed the National Model Clinical Governance Framework. The Clinical Governance Framework is based on the National Safety and Quality Health Service (NSQHS) Standards - in particular the Clinical Governance Standard and the Partnering with Consumers Standard. The Clinical Governance Framework has five components:
- Governance, leadership and culture
- Patient safety and quality improvement systems
- Clinical performance and effectiveness
- Safe environment for the delivery of care
- Partnering with consumers.
Introduction
Health care in Australia is provided by teams of clinicians working in partnership with patients, families and carers. It is delivered in a wide variety of public and private organisations, ranging from sole proprietorships to large statutory corporations and public companies.
Patients, consumers and the community trust clinicians and health service organisations to provide safe, high-quality health care, and most Australians have access to such care. Australia’s clinicians are highly regarded as skilled professionals who are committed to meeting the healthcare needs of their patients. Key safety and quality risks have been identified, and strategies exist to improve the safety and quality of health care. Although there is a strong system-wide commitment to continuous improvement, delays and problems with implementation mean that failures in safety and quality continue to occur.
Australia generally performs well in international comparisons about health.1 However, although most health care in Australia leads to good outcomes, patients do not always receive the care that is most appropriate for them, and preventable adverse events occur across the Australian healthcare system.2 Lapses in safety and quality, and unwarranted variation in health care provided to different populations within Australia have substantial costs, in terms of both the effect on people’s lives and financially.2,3
The delivery of health care is a complex endeavour. Contemporary models of care are sophisticated and rapidly changing, as are the expectations of patients and consumers. Health service organisations such as hospitals sit within intricate webs of different types of services across tertiary, secondary and primary sectors. Patients and consumers move between these services and sectors, and safety and quality risks exist at all points on these journeys.4-6
Traditionally, ensuring an acceptable standard of safety and quality was viewed as predominantly the responsibility of individual clinicians. Now, the importance of the individual and collective roles and responsibilities of patients, consumers, clinicians, healthcare teams, managers, directors, governing bodies and departments of health is well recognised. Although the safety and quality of health care provided to each patient are highly dependent on the skills and performance of individual clinicians, safety and quality are also a professional and organisational responsibility. They rely on effective governance and management processes, and the establishment of systems involving a large number of contributors in health service organisations and across the health system.
To support the delivery of safe and high-quality health care, and the best possible outcomes for patients in this complex environment, the Australian Commission on Safety and Quality in Health Care (the Commission) has developed this National Model Clinical Governance Framework (Clinical Governance Framework) for public and private healthcare organisations in the acute sector.
The Clinical Governance Framework is based on the National Safety and Quality Health Service (NSQHS) Standards (second edition), particularly the Clinical Governance Standard and the Partnering with Consumers Standard.7 As part of the complete set of NSQHS Standards, these two standards constitute a complete and robust clinical governance framework.
Purpose
The purpose of the Clinical Governance Framework is to ensure that patients and consumers receive safe and high-quality health care by describing the elements that are essential for acute health service organisations to achieve integrated corporate and clinical governance systems. Through these systems, organisations and individuals are accountable to patients and the community for continuously improving the safety and quality of their services. The Clinical Governance Framework:
- Defines clinical governance
- Provides the context for clinical governance being an integrated component of corporate governance
- Describes the key components of a clinical governance framework, based on the NSQHS Standards
- Discusses the role of culture in supporting good clinical governance
- Outlines the roles and responsibilities of, and essential partnership between, patients and consumers, clinicians, managers, and governing bodies (such as boards) in implementing effective clinical governance systems in health service organisations.
Application and use
It is mandatory for all Australian hospitals and day procedure services to be assessed through an independent accreditation process to determine whether they have implemented the NSQHS Standards. Therefore, the elements in the Clinical Governance Framework are also mandatory for these health service organisations.
As with the NSQHS Standards, the Clinical Governance Framework does not specify how a health service organisation should develop or implement its clinical governance systems. Rather, it outlines the components of a clinical governance framework to enable health service organisations to develop and implement their own governance systems, considering local needs, values and the context in which services are provided.
The Clinical Governance Framework builds on the NSQHS Standards, providing more information about corporate and clinical governance, and roles and responsibilities relating to clinical governance for people within a health service organisation.
Detailed guidance about strategies to meet the requirements of the NSQHS Standards is included in the guides for hospitals and other types of health service organisations that are currently being developed by the Commission. The Clinical Governance Framework should be used with these documents.
The Clinical Governance Framework can be used by clinicians, managers, executives, governing bodies, and state and territory departments of health to support effective clinical governance and improve the safety and quality of care.
The Clinical Governance Framework will be supported by resources developed by the Commission for specific target audiences, including members of governing bodies (such as boards), clinicians and consumers. Resources will also be developed to support application of the Clinical Governance Framework in specific settings, such as private hospitals and day procedure services.
The Clinical Governance Framework applies to public and private health services in the acute sector. As noted earlier, however, the delivery of health care in Australia is complex, and patients move between different types of services across acute and primary sectors. Because of this complexity, and the safety and quality risks that exist at these transition points4-6, there is a need to work towards an integrated system of clinical governance for the whole health system. The Clinical Governance Framework is a starting point for future work that will explore clinical governance in primary care.8
Definition of clinical governance
The definition of clinical governance that underpins the Clinical Governance Framework is as follows:
Clinical governance is the set of relationships and responsibilities established by a health service organisation between its state or territory department of health (for the public sector), governing body, executive, clinicians, patients, consumers and other stakeholders to ensure good clinical outcomes.9 It ensures that the community and health service organisations can be confident that systems are in place to deliver safe and high-quality health care, and continuously improve services.
Clinical governance is an integrated component of corporate governance of health service organisations. It ensures that everyone – from frontline clinicians to managers and members of governing bodies, such as boards – is accountable to patients and the community for assuring the delivery of health services that are safe, effective, integrated, high quality and continuously improving.
Corporate (organisational) governance of health service organisations
Clinical governance is an integrated component of corporate governance. This section provides an overview of key concepts and elements of corporate governance, particularly regarding the responsibilities of governing bodies such as boards.
Key concepts
A large proportion of Australian health care is delivered in public sector and private sector organisations governed by bodies such as boards of directors. Boards are generally well versed in the concepts and practices of corporate governance, which is recognised as a responsibility of governing bodies, and is distinguished from responsibility for management and service delivery.
The concept of clinical governance is best understood as founded in, and consistent with, broader concepts of corporate or organisational governance (in the public sector, since not all health service organisations are corporations with a governing board, the term 'organisational governance can be used, rather than 'corporate governance').
Robert Tricker is credited with creating the term ‘corporate governance’. According to Tricker10:
The governance role is not concerned with the running of the company, per se, but with giving overall direction to the enterprise, with overseeing and controlling the executive actions of management and with satisfying legitimate expectations of accountability and regulation by interests beyond the corporate boundaries.
Corporate governance encompasses the establishment of systems and processes that shape, enable and oversee management of an organisation. It is the activity, undertaken by governing bodies such as boards, of formulating strategy, setting policy, delegating responsibility, overseeing management, and ensuring that appropriate risk management and accountability arrangements are in place throughout the organisation.
Management, on the other hand, is concerned with doing – with coordinating and managing the day-to-day operations of the business.11
Responsibilities of governing bodies for corporate governance
Good governance is clearly recognised as a responsibility of governing bodies such as boards:
It is the board’s responsibility to ensure good governance and to account to [shareholders] for their record in this regard.12
Management has an operational focus, whereas governance has a strategic focus. Managers run organisations, whereas their boards ensure that organisations are run well and in the right direction.
The governing body derives its authority to conduct the business of the organisation from the enabling legislation and the organisation’s constitutional documents, where applicable. The board ‘governs’ the organisation by establishing a ‘governance system’, elements of which are implemented by the board itself, leaders and the workforce at all levels of the organisation. As part of its governance system, the governing body:
- Establishes a strategic and policy framework
- Delegates responsibility for operating the organisation to the chief executive officer, who, in turn, delegates specific responsibilities to members of the workforce
- Supervises the performance of the chief executive officer
- Monitors the performance of the organisation and ensures that there is a focus on continuous quality improvement.
The model described by Tricker for the role and functions of governance highlights both the forward-looking (leadership and performance) and retrospective (accountability and conformance) elements of good governance (Figure 1).10
The generally accepted governance duties and responsibilities of a governing body such as a board include:
- Appointing a chief executive officer, supporting them to lead the organisation and evaluating their performance
- In consultation with management, setting and reviewing organisational plans and strategies
- Endorsing and approving budgets, and major financial and organisational decisions
- Ensuring that the organisation is being properly managed, including that
- systems of production or service delivery are well designed and fit for purpose
- services meet desired standards
- the organisation meets its compliance obligations
- Challenging the assumptions of management
- Reviewing and monitoring performance of the control framework to ensure that major risks are identified and managed
- Ensuring that there is an ongoing focus on quality improvement
- Evaluating reports, and reviewing feedback, suggestions and complaints
- Ensuring the continuing development of the executive management team
- Planning for succession
- Communicating with, and being accountable to, internal and external stakeholders.
Although it is ultimately the governing body’s responsibility to ensure good corporate governance, many governance responsibilities are distributed throughout the organisation. For example, people at all levels of a health service organisation help to design and implement risk management, performance monitoring and audit programs, which are key elements of good governance systems. It is the board’s responsibility, however, to ensure that the overall governance system is implemented effectively, and that the board is accountable for the outcomes and performance of the organisation.
Clinical governance and the National Model Clinical Governance Framework
This section describes how clinical governance is an integrated component of broader corporate governance and sets out the key elements of the Clinical Governance Framework, based on the NSQHS Standards.
Clinical governance as an integrated component of organisational governance
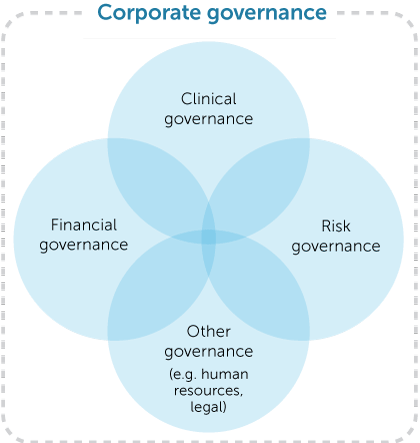
The responsibility of a governing body such as a board for clinical governance is an integrated element of its overall responsibility and accountability to govern the organisation (Figure 2). As a component of broader systems for corporate governance, clinical governance involves a complex set of leadership behaviours, policies, procedures, and monitoring and improvement mechanisms that are directed towards ensuring good clinical outcomes.
The clinical governance system of a health service organisation therefore needs to be conceptualised as a system within a system – a clinical governance system within a corporate governance system.
Under this model, it is important to recognise the following:
- Clinical governance is of equivalent importance to financial, risk and other business governance
- Decisions about other aspects of corporate governance can have a direct affect on the safety and quality of care, and decisions about clinical care can have a direct affect on other aspects of corporate governance, such as financial performance and risk management
- Governing bodies are ultimately responsible for good corporate (including clinical) governance
- Governing bodies cannot govern clinical services well without the deep engagement of skilled clinicians working at all levels of the organisation
- Clinicians, managers and members of governing bodies have individual and collective responsibilities for ensuring the safety and quality of clinical care; as well as being reflected in the NSQHS Standards, many of these responsibilities are specified in relevant professional codes of conduct.
Although it is ultimately the responsibility of a governing body to set up a sound clinical governance system, and be accountable for outcomes and performance within this system, implementation involves contributions by individuals and teams at all levels of the organisation. There is also reliance on well-designed systems that deliver, monitor and account for the safety and quality of patient care.
The application of clinical governance systems to achieve good clinical outcomes requires a focus on both what happens within a health service organisation, and the integration and linkages of the health service organisation within a network of other health service organisations in the acute and primary care sectors. This network may include general practitioners, other specialists, allied health providers and aged care homes.
Components of the Clinical Governance Framework
The Clinical Governance Framework is based on the NSQHS Standards (2nd ed.) – in particular, the Clinical Governance Standard and the Partnering with Consumers Standard.
The NSQHS Standards were developed by the Commission in consultation and collaboration with states and territories, the private sector, executives and managers, clinical experts, patients, and carers. The primary aims of the NSQHS Standards are to protect the public from harm and to improve the quality of health service provision. Since 2013, it has been mandatory for all Australian hospitals and day procedure services to be assessed through an independent accreditation process to determine whether they have implemented the NSQHS Standards.
To fully apply the NSQHS Standards in a health service organisation, governing bodies, management, patients, consumers, clinicians and clinical teams need to be engaged in the implementation of actions set out in the NSQHS Standards.
In the context of the complete set of NSQHS Standards, the Clinical Governance Standard and the Partnering with Consumers Standard together ensure the creation of clinical governance systems within healthcare organisations that:
- Are fully integrated within overall corporate governance systems
- Are underpinned by robust safety and quality management systems
- Maintain and improve the reliability, safety and quality of health care
- Improve health outcomes for patients.
To achieve a complete and robust clinical governance system, actions to meet the Clinical Governance Standard and the Partnering with Consumers Standard need to be supported by actions to meet the other six NSQHS Standards.
As reflected in the NSQHS Standards, the Clinical Governance Framework has five components (Figure 3). The central component relates to patients and consumers, who are at the centre of the Clinical Governance Framework. The five components of the Clinical Governance Framework are as follows:
| Governance, leadership and culture | Integrated corporate and clinical governance systems are established, and used to improve the safety and quality of health care for patients |
|---|---|
| Patient safety and quality improvement systems | Safety and quality systems are integrated with governance processes to actively manage and improve the safety and quality of health care for patients |
| Safe environment for the delivery of care | The environment promotes safe and high-quality health care for patients |
| Partnering with consumers |
Systems are designed and used to support patients, carers, families and consumers to be partners in healthcare planning, design, measurement and evaluation; elements of this component include
|
Detailed information about each component of the Clinical Governance Framework, including strategies for improvement, is available in the guides developed by the Commission to support the NSQHS Standards.
The actions specified in the NSQHS Standards for the Clinical Governance Standard and the Partnering with Consumers Standard are in the Appendix. These actions comprise the Clinical Governance Framework.
Importance of culture in clinical governance
The NSQHS Standards specify the actions that a health service organisation needs to take to develop and set up systems for good clinical governance. Culture, however, is just as important in clinical governance in ensuring that patients and consumers receive safe and high-quality care.
Culture is a complex and contested concept that has many different definitions. Central to most of these definitions is that culture consists of:
… the values, beliefs and assumptions shared by occupational groups. These shared ways of thinking are then translated into common and repeated patterns of behaviour: patterns of behaviour that are in turn maintained and reinforced by the rituals, ceremonies and rewards of everyday organisational life.13
Factors that have been identified as being important for sustaining cultures that ensure safe and high-quality care include14-15:
- Leaders articulating a vision for high-quality, compassionate and safe care, and acting on this vision throughout the organisation
- Translating the vision into clear objectives for safety and quality at all levels of the organisation, and establishing measures to assess progress
- Providing a supportive and positive working environment for the workforce
- Ensuring that members of the workforce are engaged in their work
- Having an organisation that is transparent about performance, open to learning and continuously improving
- Supporting multidisciplinary teams to work together effectively.
To put in place the requirements of the NSQHS Standards that are the basis of the Clinical Governance Framework, health service organisations need to have a culture that has16:
- Strong strategic and cultural leadership of clinical services, focusing on
- effective planning to enable development and improvement opportunities to be captured
- cultural leadership that requires, and gives priority to, safety and quality, and supports continuous improvement
- allocating resources to support the delivery of high-quality care
- Clear responsibilities for managing the safety and quality of care, and delegation of the necessary management authority for this purpose
- Reliable processes for ensuring that systems for delivery of care are designed and performing well, and clinicians are fully engaged in the design, monitoring and development of these systems
- Effective use of data and information to monitor and report on performance, through the health service organisation to the governing body
- Well-designed systems for identifying and managing clinical risk.
Roles and responsibilities for clinical governance
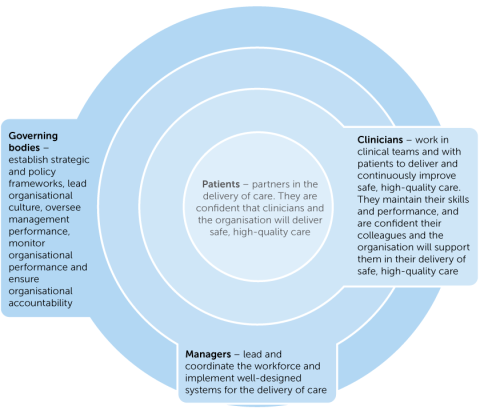
Good clinical governance provides confidence to the community and everyone who works in a health service organisation that systems are in place to support the delivery of safe, high-quality health care. Within a well-governed healthcare organisation, everyone, including frontline clinicians, managers and the governing body, is accountable for their contribution to the safety and quality of care delivered to patients. Broadly, these roles are as follows (Figure 4):
| Patients and consumers | Patients and consumers participate as partners to the extent that they choose. These partnerships can be in their own care, and in organisational design and governance. |
|---|---|
| Clinicians | Clinicians work within, and are supported by, well-designed clinical systems to deliver safe, high-quality clinical care. Clinicians are responsible for the safety and quality of their own professional practice, and professional codes of conduct include requirements that align with the Clinical Governance Framework.17 |
| Managers | Managers (including clinical managers) advise and inform the governing body, and operate the organisation within the strategic and policy parameters endorsed by the governing body. They are primarily responsible for ensuring that the systems that support the delivery of care are well designed and perform well. |
| Governing body | The governing body is ultimately responsible for ensuring that the organisation is run well and delivers safe, high-quality care. It does this by establishing a strong safety culture through an effective clinical governance system, satisfying itself that this system operates effectively, and ensuring that there is an ongoing focus on quality improvement. |
In addition to these roles, state and territory departments of health provide centralised and coordinated oversight of the performance of health service organisations, and create a common set of safety metrics that report meaningful safety and quality outcomes.
Implementation of an organisation’s clinical governance system involves contributions by individuals and teams at all levels of the organisation. Roles and responsibilities for clinical governance at all levels of the system are summarised in the following sections.
References
- Organisation for Economic Co-operation and Development. Health at a glance: OECD indicators. Paris: OECD; 2013.
- Australian Commission on Safety and Quality in Health Care. Vital signs 2015: the state of safety and quality in Australian health care. Sydney: ACSQHC; 2015.
- Harrison R, Walton M, Manias E, Mears S, Plumb J. Patients’ experiences in Australian hospitals: a systematic review of evidence. Aust Health Rev 2016;41:419–35.
- Australian Commission on Safety and Quality in Health Care. Draft National Safety and Quality Health Service Standards, version 2. Sydney: ACSQHC; 2016.
- Cummings E, Showell C, Roehrer E, Churchill B, Turner B, Yee KC, et al. Discharge, referral and admission: a structured evidence-based literature review. eHealth Services Research Group, University of Tasmania (on behalf of the Australian Commission on Safety and Quality in Health Care, and the NSW Department of Health); 2010.
- Witherington E, Pirzada O, Avery A. Communication gaps and readmissions to hospital for patients aged 75 years and older: observational study. Qual Saf Health Care 2008;17:71–5.
- Russell L, Doggett J, Dawda P, Wells R. Patient safety – handover of care between primary and acute care: policy review and analysis. Prepared for the National Lead Clinicians Group by the Australian Primary Health Care Research Institute, Australian National University. Canberra: National Lead Clinicians Group, Australian Government Department of Health and Ageing; 2013.
- Jones, A, Killion S. Clinical governance for Primary Health Networks. Canberra: Deeble Institute; 2017.
- Australian Commission on Safety and Quality in Health Care. National Safety and Quality Health Service Standards. Sydney: ACSQHC; 2011.
- Tricker RI. Corporate governance: practices, procedures, and powers in British companies and their boards of directors. London: Gower; 1984.
- Edwards M, Clough R. Corporate governance and performance: an exploration of the connection in a public sector context. Canberra: University of Canberra; 2005. (Issues Series Paper No. 1.)
- Committee on Corporate Governance. Final report. London: Committee on Corporate Governance; 1988.
- Davies HTO, Mannion R. Will prescriptions for cultural change improve the NHS? BMJ 2013;346:f1305.
- West MA. Creating a culture of high-quality care in health services. Global Economics and Management Review 2013;18:40–4.
- West MA, Lyubovnikova J, Eckert R, Denis JL. Collective leadership for cultures of high quality health care. JOEPP 2014;1:240–60.
- Australian Commission on Safety and Quality in Health Care. Safety and quality improvement guide – Standard 1: Governance for safety and quality in health service organisations. Sydney: ACSQHC; 2012.
- Medical Board of Australia. Good medical practice: a code of conduct for doctors in Australia. Melbourne: MBA; 2014.
